Mental illness affects nearly 800 million people worldwide – yet there are still many misconceptions about what it means to have a mental disorder. Unfortunately, many individuals don’t receive proper care or treatment due to these misunderstandings. It makes access to reliable resources like the DSM-5 even more vital to ensure those suffering from a medical condition get the proper diagnosis.
The American Psychiatric Association revised DSM-4 to DSM-5 in 2013 and DSM-5 TR in 2022. It’s an authoritative guidebook for clinicians worldwide to diagnose and classify mental health disorders. The manual is regularly updated with new research findings on conditions such as anxiety, depression, bipolar disorder, schizophrenia, etc., ensuring medical professionals stay up-to-date with current best practices for identifying and managing mental illnesses. By further reading this article, you will better understand how the DSM 5 TR supports those with a mental illness.
What Is The Purpose Of The Dsm 5?
The DSM 5 TR provides diagnostic codes for clinicians to identify various mental illnesses and includes information about changes since its last publication (March 2022). Despite being criticized by some as having shortcomings or lacking accuracy, it remains one of the most widely used resources for differential diagnosis among psychiatric medical professionals worldwide.
The book is a manual to clinical practice and should not be seen as providing absolute truth or certainty when diagnosing a patient’s medical condition. Instead, it is an additional tool in helping medical practitioners make informed decisions on how best to treat their patients with mental illness. Furthermore, many other countries use different versions of the International Classification of Diseases (ICD). ICD also helps with mental illness diagnoses. While there are differences between these two manuals, they both serve similar purposes – to help health workers accurately diagnose mental health conditions so that appropriate treatment can be provided.
How Was The Dsm-5 Content Created?
To create the DSM-5, hundreds of experts worldwide contributed their knowledge on various mental health diagnoses and treatment topics. It included contributions from psychiatrists, psychologists, social workers, researchers, patient advocates, and more. These contributors provided information about different aspects of each mental health disorder, such as prevalence rates, symptoms associated with each disorder, risk factors linked to it, etc. It has helped American Psychiatric Association to develop descriptions for these disorders. Additionally, they consulted recent research findings regarding new or emerging mental disorders like Anxiety Disorders, Personality Disorders, and Other Psychotic Disorders, as well as Suicidal Behavior and Binge Eating Disorder.
The collective effort ensured that all the information needed for accurate mental health diagnosis was available in one volume – the DSM 5 TR. It makes DSM 5 TR a helpful resource for professionals in diagnosing and treating people with a mental disorders.
What Areas Does The DSM 5 TR Cover?
The manual provides detailed diagnostic criteria for clinicians to accurately assess each patient’s presenting symptoms. The DSM 5 TR has been updated from its previous version with new information about conditions such as depression, anxiety disorders, bipolar disorder, and schizophrenia. It also includes updates on other common mental disorders, including attention deficit hyperactivity disorder (ADHD), obsessive-compulsive disorder (OCD), posttraumatic stress disorder (PTSD), gambling disorder, and substance use disorders. In addition, it guides how to distinguish between different types of mental disorders. The DSM-5 is divided into three sections.
- DSM-5 Basics guides healthcare professionals on how to use the manual in their practice. This section also includes instructions on using the DSM-5 in situations involving legal professionals or court cases.
- Diagnostic Criteria and Codes is the most extensive section of the manual. Each chapter in this section focuses on a specific type of condition and provides detailed explanations and definitions of individual disorders.
- Emerging Measures and Models contain information about specific assessment tools that healthcare providers use to diagnose certain conditions. This section also includes information on how cultural differences may affect a diagnosis and a chapter on situations that require further study before being added to a later edition of the DSM.
The DSM-5 is used by practitioners worldwide, specializing in diagnosing and treating mental health conditions. Its comprehensive coverage is essential in providing reliable diagnoses and understanding treatments tailored to individual patients’ needs. By utilizing this resource, a mental health professional can better understand the complexities surrounding various mental illnesses and create informed plans for care that will allow individuals to achieve optimal outcomes. With its rigorous standards for accuracy and thoroughness, the DSM-5 is a valuable tool for clinical practice and research into mental health issues. Transitioning now onto DSM-5 Section II: Diagnostic Criteria & Code.
Dsm 5 – Diagnostic Criteria And Code
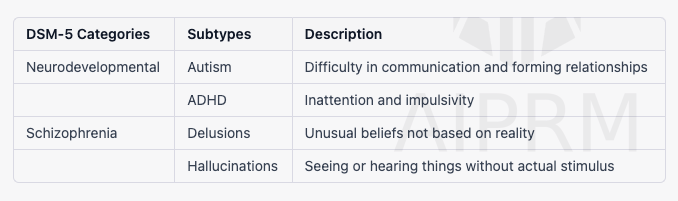
DSM 5 offers a diagnostic framework that allows practitioners to classify mental health disorders and provide clinical diagnoses accurately. In Section II of the DSM-5, Diagnostic Criteria and Code are outlined in detail; see the table below. The section provides diagnostic criteria for each disorder.
| Category | Examples of Disorders |
| Neurodevelopmental Disorders | Autism spectrum disorder, ADHD, learning disorders |
| Schizophrenia Spectrum and Other Psychotic Disorders | Schizophrenia, schizoaffective disorder, delusional disorder |
| Bipolar and Related Disorders | Bipolar I and bipolar II disorders, cyclothymic disorder |
| Depressive Disorders | Major depressive disorder, persistent depressive disorder |
| Anxiety Disorders | Generalized anxiety disorder, panic disorder, phobias |
| Obsessive-Compulsive and Related Disorders | Obsessive-compulsive disorder, hoarding disorder, body dysmorphic disorder |
| Trauma- and Stressor-Related Disorders | PTSD, acute stress disorder, adjustment disorder |
| Dissociative Disorders | Dissociative identity disorder, dissociative amnesia, depersonalization/derealization disorder |
| Disruptive, Impulse-Control, and Conduct Disorders | Somatic symptom disorder, illness anxiety disorder, functional neurological symptom disorder |
| Eating and Feeding Disorders | Anorexia nervosa, binge-eating disorder, bulimia nervosa |
| Sleep-Wake Disorders | Insomnia disorder, narcolepsy, restless legs syndrome |
| Sexual Dysfunctions | Sexual dysfunctions, gender dysphoria-related disorders |
| Gender Dysphoria | Gender dysphoria-related disorders |
| Disruptive, Impulse-Control and Conduct Disorders | Antisocial personality disorder, kleptomania, oppositional defiant disorder |
| Substance-Related and Addictive Disorders | Alcohol use disorder, inhalant use disorder, opioid use disorder, gambling disorder |
| Neurocognitive Disorders | Alzheimer’s disease, delirium, Parkinson’s disease, traumatic brain injury |
| Personality Disorders | Borderline personality disorder, narcissistic personality disorder |
| Paraphilic Disorders | Sexual behavior disorders |
| Other Mental Disorders and Additional Codes | Somatic Symptoms and Related Disorders |
| Medication-Induced Movement Disorders and Other Adverse Effects of Medication | Tardive dyskinesia, neuroleptic malignant syndrome |
| Other Conditions That May Be a Focus of Clinical Attention | Self-harm and suicidal behaviors, unemployment, a history of any type of abuse |
The section provides precise definitions for each disorder and associated symptomology. Not only does it offer clear descriptions of symptoms, but it also outlines potential causes of distress or impairment related to the disorder being diagnosed. Additionally, it includes helpful information on epidemiology, cultural considerations when diagnosing certain disorders, differentials based on age group, gender differences in presenting symptoms, and other pertinent details relevant to making a confident clinical diagnosis.
DSM-5, Diagnostic Criteria, and Code is a resource that helps clinicians arrive at accurate conclusions regarding a patient’s condition. With its detailed summaries and up-to-date guidelines, Section II provides essential guidance for making reliable diagnoses and determining appropriate interventions for managing mental health issues. I
With its comprehensive approach to outlining diagnostic classification and code criteria, Section II readily equips clinicians with all they need to make informed decisions that lead to elimination disorders. Combining clarity with precision in describing signs, symptom codes, and treatment suggestions for various conditions, the DSM 5 ensures that providers have the fundamental knowledge required to deliver quality care in today’s dynamic healthcare environment.
How Does A Clinician Use Dsm-5?
The manual contains descriptive criteria for different diagnoses and guides on accurately assessing mental illnesses.
To use the DSM-5 effectively, clinicians must first understand its basic structure. The manual is organized into five categories: Neurodevelopmental Disorders, Schizophrenia Spectrum and Other Psychotic Disorders, Bipolar and Related Disorders, Depressive Disorders, Anxiety Disorders, and Obsessive Compulsive Disorder (OCD). Within each category are multiple subtypes that describe various symptoms associated with a particular disorder. Clinicians can then compare these descriptions against their patient’s behavior or psychiatric history to make a diagnosis.
The information allows healthcare providers to gain insight into their patients’ behaviors and develop appropriate treatment plans accordingly. Additionally, since many diagnostic tools are available within the DSM-5 beyond just categorizing mental illness, clinicians may also utilize them when evaluating other aspects of a patient’s mental disorder, such as cognitive abilities or personality traits. It helps them create customized care plans tailored specifically to the individual needs of each patient they treat.
By providing clear definitions of different types of mental illnesses and helping clarify any confusion about symptomatology or diagnosis, the DSM-5 has become an invaluable tool for both established practitioners and those new to the field of psychiatry. Its importance cannot be overstated; it forms the basis for much of our understanding of mental health disorders—and will continue to do so well into the future.
FAQ
What is the DSM-5 in simple terms?
The DSM-5 is a book that helps doctors and other professionals understand different mental health conditions. It provides a common language for mental health professionals to describe and diagnose these conditions. The book is divided into sections, each covering a different type of condition, such as autism, depression, anxiety, and more. For each condition, the book provides clear descriptions of the symptoms, criteria for diagnosis, and recommended treatments. The DSM-5 is important for helping people get the care they need to live healthy and happy life.
How does the DSM-5 TR define mental disorders?
The DSM-5 defines a mental disorder as a syndrome that involves a clinically significant disturbance in an individual’s thoughts, emotions, or behaviors. The disruption must reflect a dysfunction in the psychological, biological, or developmental processes underlying mental functioning. Additionally, the disorder must be associated with distress, disability, or an increased risk of suffering or harm to oneself or others. The DSM-5 also notes that a mental disorder is not a culturally specific reaction to an event, such as grief, and is not primarily a result of social deviance or societal conflicts. Instead, a mental disorder is a clinically significant condition that requires assessment and intervention by trained mental health professionals.
Are There Any Alternatives To The DSM-5 TR?
One option for people seeking an alternative to DSM 5 is the International Classification of Diseases (ICD) system, published by the World Health Organization (WHO). The ICD provides a comprehensive list of medical diagnoses and treatments from across the globe, which can help clinicians identify patients’ disorders more accurately than using only one country’s diagnostic manual. Additionally, it offers helpful information on treating certain conditions that might not be available in other manuals.
Another possible alternative is the Multiaxial System of Psychiatric Diagnosis created by psychiatrists at Johns Hopkins University School of Medicine. The multiaxial system involves assessing multiple factors when identifying psychiatric illness – including biological, psychological, social, environmental, and cultural influences – rather than relying solely on symptoms as with traditional DSM approaches. This approach has been found to provide more accurate diagnosis results than single-axis systems like the DSM-5.
For people seeking a non-medical perspective on diagnosing mental illness, self-reporting questionnaires may offer insight into someone’s individual experience with their condition. These instruments typically include questions about specific behaviors and feelings associated with different disorders, allowing individuals to gain greater awareness about themselves without relying on professional assessment tools such as the DSM-5.
What Is The Difference Between The Dsm-5 And Icd-10?
To cut to the chase, there is a significant distinction between the DSM-5 and ICD-10. On the surface level, they both serve as diagnostic manuals for health professionals — but that’s where the similarities end. The DSM-5 is mainly used in America, while the ICD-10 is used globally.
The key difference between these two systems lies in their approach. While the DSM-5 focuses on describing and classifying symptoms, the ICD-10 takes a more detailed look at each disorder by providing codes for further medical data analysis. It means that psychiatrists can use ICD-10 to break down diagnoses into smaller components and provide precise treatment plans tailored to each patient’s needs.
Additionally, another point worth considering when comparing them is their scope; At the same time, the DSM-5 covers most disorders seen in clinical settings; it does not include certain rare conditions or diseases outside its domain, such as some neurological disorders— something which makes it difficult for clinicians if they come across cases involving those illnesses. In comparison, ICD-10 provides comprehensive coverage with far fewer limitations due to its expansive database of codes and varying levels of complexity. One could say that ICD-10 offers a much broader range of applications than what you would find with the DSM-5, making it an invaluable tool in any clinician’s arsenal.
So, although both systems have roughly similar purposes – namely, diagnosing mental illness – they differ significantly based on how specific or broad their diagnosis criteria are and how much detail goes into breaking down individual cases.
Conclusion
In conclusion, the DSM-5 is a diagnostic and statistical manual for clinicians to diagnose mental disorders. The DSM 5 TR has been updated from previous versions, focusing on clarity and accuracy. It is revised periodically by experts in the field; however, it does not replace all prior versions. For those seeking alternatives to the DSM-5, there is the ICD-10 which can provide additional information about the diagnosis.
The differences between these two classification systems are significant, but both have their strengths. The DSM-5 provides more detailed descriptions that are easier to understand, while ICD-10 offers greater granularity regarding symptoms and risk factors. With so much at stake when diagnosing mental disorders, having access to both resources can be valuable for professionals who want to make accurate diagnoses and provide effective treatment plans.
Overall, one thing remains clear: the DSM-5 is a powerful diagnostic resource that should not be taken lightly or dismissed as outdated technology – it will continue to evolve as medical science advances, allowing clinicians to serve their patients better using cutting-edge tools and techniques. In this day and age, where mental illness remains largely misunderstood and stigmatized, accurately identifying disorders through evidence-based practices is paramount in helping individuals achieve optimal wellness outcomes.
 English
English Español
Español Français
Français Português
Português Svenska
Svenska